Pink eye, or conjunctivitis, is a common eye condition known for its redness, itching, and discharge. However, these symptoms are not unique to conjunctivitis. Several other eye conditions can mimic these signs, leading to frequent misdiagnoses.
This article explores six other issues often mistaken for pink eye, helping you understand and identify these conditions for accurate treatment.
1. Allergies
Allergies can often be mistaken for pink eye due to the overlap in symptoms, such as redness, itching, and watery eyes. Allergic conjunctivitis is specifically triggered by allergens like pollen, dust mites, pet dander, mold, and other environmental factors. Here’s a detailed explanation of everything related to this topic:
Causes

Allergic conjunctivitis occurs when the eyes react to allergens, substances that the immune system identifies as harmful, even though they are usually harmless. Common allergens include:
- Pollen: Often from trees, grass, and weeds, pollen is a major trigger during certain seasons, like spring and fall.
- Dust mites: These tiny creatures live in household dust and thrive in bedding, upholstery, and carpets.
- Pet dander: Proteins found in the skin flakes, urine, and saliva of furry pets like cats and dogs.
- Mold: Spores from mold can be found both indoors and outdoors and can cause year-round symptoms.
Symptoms
The symptoms of allergic conjunctivitis can vary in severity but generally include:
- Redness: Caused by the dilation of blood vessels in the conjunctiva.
- Itching: Often intense and can lead to further irritation from rubbing the eyes.
- Watery eyes: Increased tear production in response to the allergen.
- Swelling: Puffiness around the eyes can occur, particularly on the eyelids.
- Burning sensation: A feeling of heat or discomfort in the eyes.
- Photophobia: Sensitivity to light is common in more severe cases.
Diagnosis
Diagnosing allergic conjunctivitis involves a combination of patient history, symptom observation, and sometimes specific tests. Eye care professionals may:
- Conduct a physical examination: Checking the eyes for redness, swelling, and discharge.
- Review medical history: Looking for a history of allergies or related conditions like eczema or asthma.
- Perform allergy tests: Skin prick tests or blood tests can identify specific allergens causing the reaction.
Treatment
Treating allergic conjunctivitis focuses on relieving symptoms and avoiding allergens. Common treatments include:
- Antihistamines: Oral or topical antihistamines help reduce itching, redness, and swelling by blocking histamine, a chemical released during an allergic reaction.
- Decongestants: These can help reduce redness by narrowing blood vessels in the eyes.
- Mast cell stabilizers: Used to prevent the release of chemicals that cause allergic reactions.
- Corticosteroids: For severe cases, corticosteroid eye drops may be prescribed to reduce inflammation.
- Avoidance strategies: Minimizing exposure to known allergens, such as using air purifiers, washing bedding frequently, and keeping pets out of certain areas of the home.
Prevention
Preventing allergic conjunctivitis involves both avoiding known allergens and taking proactive steps to reduce exposure:
- Keep windows closed during high pollen seasons.
- Use air conditioning instead of opening windows.
- Regularly clean and dust your home to reduce dust mites.
- Wash hands after petting animals and avoid touching your face.
- Use allergen-proof bedding covers.
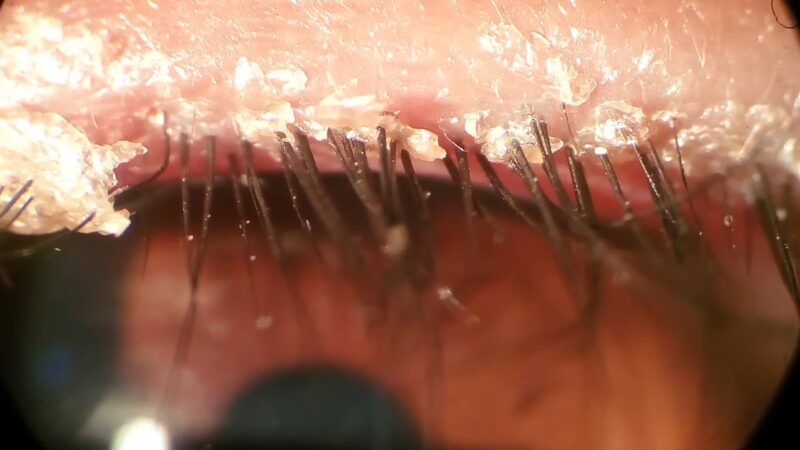
2. Blepharitis
Blepharitis is another condition frequently mistaken for pink eye due to the overlap in symptoms such as redness, itching, and irritation. It involves inflammation of the eyelids, often affecting the part where the eyelashes grow and sometimes the inner edge of the eyelid. Here’s everything you need to know about blepharitis:
Causes
Blepharitis can be caused by several factors, including:
- Bacterial infections: Staphylococcus bacteria are commonly involved.
- Seborrheic dermatitis: A skin condition that affects the scalp, eyebrows, and eyelids.
- Rosacea: A skin condition that causes redness and pimples.
- Allergies: Reactions to environmental allergens or eye makeup.
- Mite infestation: Tiny mites like Demodex can live in the hair follicles and cause irritation.
Symptoms
Symptoms of blepharitis can be chronic and may include:
- Redness: Especially noticeable on the eyelid margins.
- Swelling: Puffiness of the eyelids.
- Itching: Persistent and often leading to further irritation from rubbing.
- Crusty eyelashes: Especially upon waking, with flaky skin or dandruff-like scales.
- Burning sensation: A feeling of heat or discomfort in the eyes.
- Tearing: Increased tear production.
- Photophobia: Sensitivity to light.
- Dry eyes: A gritty or sandy feeling in the eyes.
- Eyelid sticking: Particularly in the morning.
Diagnosis
Diagnosing blepharitis involves a thorough examination by an eye care professional:
- Eye examination: Using a magnifying instrument to examine the eyelids and the base of the eyelashes.
- Medical history review: Checking for related conditions like rosacea or seborrheic dermatitis.
- Lid margin swab: Sometimes a sample is taken to check for bacteria or mites.
Treatment
Treatment focuses on managing symptoms and maintaining eyelid hygiene:
- Warm compresses: Applied to the eyelids to loosen crusts and improve oil gland function.
- Eyelid scrubs: Using diluted baby shampoo or commercial lid cleansers to clean the eyelid margins.
- Antibiotics: Topical antibiotics like erythromycin or oral antibiotics for more severe cases.
- Steroid eye drops or ointments: To reduce inflammation.
- Artificial tears: To relieve dry eye symptoms.
- Omega-3 supplements: These may help improve oil gland function in the eyelids.
Prevention
Preventing blepharitis involves regular eyelid hygiene and addressing underlying conditions:
- Maintain eyelid cleanliness: Regularly clean the eyelid margins with warm water and mild cleansers.
- Manage skin conditions: Treat underlying issues like rosacea or seborrheic dermatitis.
- Avoid eye makeup: Especially if it triggers irritation.
- Use hypoallergenic products: Reduce exposure to potential allergens.
3. Styes
Styes are another eye condition that can easily be confused with pink eye due to similar symptoms like redness and discomfort. A stye, also known as a hordeolum, is a small, painful lump on the inside or outside of the eyelid caused by a bacterial infection. Here’s a detailed look at styles:
Causes

Styes are typically caused by bacterial infections, specifically Staphylococcus bacteria. These bacteria can infect the oil glands in the eyelids, leading to the development of a stye. Factors that increase the risk of developing a stye include:
- Poor eyelid hygiene: Not cleaning the eyelids regularly.
- Touching the eyes with unwashed hands: Introducing bacteria to the eyelids.
- Using old or contaminated cosmetics: Sharing makeup or using expired products.
- Chronic conditions: Conditions like blepharitis and rosacea can contribute to the development of styes.
Symptoms
The symptoms of a stye can be quite distinct, although they share some similarities with pink eye:
- Redness: Around the affected area of the eyelid.
- Swelling: Localized to a small area of the eyelid, forming a bump.
- Pain: Often intense and localized to the site of the stye.
- Tenderness: The area around the stye may be sensitive to touch.
- Crusting: Yellowish discharge that can crust over.
- Watery eyes: Increased tear production.
- Droopy eyelid: The eyelid may droop over the stye due to swelling.
- Pus drainage: In some cases, the style may burst, releasing pus.
Diagnosis
Diagnosis of a stye is typically straightforward and involves:
- Physical examination: A healthcare provider examines the eyelid to identify the characteristic bump.
- Patient history: Review any underlying conditions or recent activities that might have contributed to the stye.
Treatment

Treatment for styes focuses on alleviating symptoms and addressing the infection:
- Warm compresses: Applying a warm, damp cloth to the eyelid several times a day can help the stye drain naturally.
- Eyelid hygiene: Keeping the eyelids clean with mild soap and water or specialized eyelid cleansers.
- Avoiding makeup: Refraining from using eye makeup until the stye heals.
- Over-the-counter pain relievers: To manage pain and reduce swelling.
- Antibiotic ointments or drops: In some cases, a doctor may prescribe antibiotics if the stye does not improve with home care.
- Surgical drainage: For severe or persistent styes, a healthcare provider may need to lance and drain the stye.
Prevention
Preventing styes involves maintaining good eyelid hygiene and avoiding behaviors that introduce bacteria to the eyes:
- Regular eyelid cleaning: Using gentle cleansers to clean the eyelids daily.
- Hand hygiene: Washing hands thoroughly before touching the face or eyes.
- Avoiding old or shared cosmetics: Not sharing makeup and replacing products regularly.
- Managing underlying conditions: Treating chronic conditions like blepharitis or rosacea to reduce the risk of styes.
4. Iritis
Iritis, or anterior uveitis, is inflammation of the iris, the colored part of the eye. It can be easily mistaken for pink eye due to similar symptoms such as redness and discomfort. Here’s a comprehensive look at iritis:
Causes

Iritis can be caused by various factors, and often the exact cause is unknown. Some common causes include:
- Autoimmune disorders: Conditions like ankylosing spondylitis, rheumatoid arthritis, and sarcoidosis can cause iritis.
- Infections: Bacterial, viral, fungal, or parasitic infections can lead to iritis.
- Trauma: Injury to the eye can result in inflammation.
- Genetic predisposition: Individuals with certain genetic markers, such as HLA-B27, are more susceptible.
- Systemic inflammatory diseases: Conditions like Crohn’s disease and ulcerative colitis.
Symptoms
The symptoms of iritis can be similar to pink eye but often involve deeper eye structures and can be more severe:
- Redness: Often concentrated around the iris rather than the entire eye.
- Pain: Especially when exposed to bright light (photophobia).
- Blurred vision: Vision may be cloudy or reduced.
- Small or irregular pupil: The affected eye’s pupil may appear smaller or oddly shaped.
- Tearing: Increased tear production.
- Headache: Pain that can extend to the brow area.
Diagnosis
Diagnosis of iritis requires a thorough examination by an eye care professional:
- Slit-lamp examination: A specialized microscope is used to examine the inside of the eye.
- Medical history: Review of any underlying conditions or recent illnesses.
- Eye pressure test: Measuring the pressure inside the eye to rule out glaucoma.
- Blood tests or imaging: In some cases, tests may be needed to identify underlying systemic conditions.
Treatment
Treating iritis focuses on reducing inflammation and addressing the underlying cause:
- Steroid eye drops: To reduce inflammation and pain.
- Dilating eye drops: To prevent muscle spasms in the iris and reduce pain.
- Oral medications: In severe cases, oral steroids or immunosuppressive drugs may be needed.
- Treating underlying conditions: Managing systemic diseases that may be causing iritis.
Prevention
Preventing iritis involves managing underlying health conditions and protecting the eyes from injury:
- Regular medical check-ups: To monitor and manage autoimmune or systemic inflammatory diseases.
- Eye protection: Using safety glasses to prevent eye injuries.
- Prompt treatment: Seeking immediate medical attention for eye infections or injuries.
5. Keratitis
Keratitis is an inflammation of the cornea, the clear, dome-shaped surface that covers the front of the eye. It can be mistaken for pink eye due to similar symptoms, but keratitis is often more severe and requires different treatment. Here’s an in-depth look at keratitis:
Causes

Keratitis can be caused by various factors, including:
- Infections: Bacterial, viral (such as herpes simplex), fungal, and parasitic infections can all lead to keratitis.
- Injury: Any injury to the cornea, including scratches or foreign bodies, can cause inflammation.
- Contact lens use: Improper care, extended wear, or contaminated contact lenses are common causes.
- Dry eye: Severe dry eye can damage the cornea and lead to keratitis.
- Contaminated water: Exposure to contaminated water, such as in hot tubs or swimming pools, can introduce harmful microorganisms.
Symptoms
Symptoms of keratitis are often more severe and can include:
- Redness: Intense redness in the affected eye.
- Pain: Significant eye pain and discomfort.
- Tearing: Excessive tear production.
- Blurred vision: Reduced clarity of vision.
- Photophobia: Sensitivity to light.
- Foreign body sensation: Feeling like something is in the eye.
- Discharge: Depending on the type of infection, discharge may be present.
Diagnosis
Diagnosing keratitis involves a thorough examination by an eye care professional:
- Slit-lamp examination: This allows the doctor to see the extent and depth of the inflammation.
- Corneal scraping: A sample from the cornea may be taken to identify the cause of the infection.
- Fluorescein staining: This dye helps highlight any corneal damage or ulceration.
Treatment
Treatment of keratitis depends on the cause and severity:
- Antibiotic eye drops: For bacterial infections.
- Antiviral eye drops: For viral infections such as herpes simplex.
- Antifungal eye drops: For fungal keratitis.
- Antiparasitic treatment: For parasitic infections, such as Acanthamoeba.
- Steroid eye drops: To reduce inflammation, but only under strict medical supervision.
- Pain relievers: To manage discomfort.
- Corneal transplant: In severe cases where the cornea is extensively damaged.
Prevention
Preventing keratitis involves proper eye care and hygiene:
- Proper contact lens care: Clean and store lenses correctly, avoid wearing them overnight, and replace them as recommended.
- Eye protection: Use goggles when swimming and avoid contaminated water sources.
- Treat underlying conditions: Manage dry eye and other conditions that can lead to keratitis.
- Avoid eye injuries: Take precautions to prevent trauma to the eyes.
6. Dry Eye Syndrome
Dry eye syndrome, also known as keratoconjunctivitis sicca, is a condition where the eyes do not produce enough tears or produce poor-quality tears. It is often mistaken for pink eye due to similar symptoms like redness, irritation, and discomfort. Here’s an extensive overview of dry eye syndrome:
Causes
Dry eye syndrome can be caused by a variety of factors, including:
- Age: Tear production tends to diminish with age.
- Environmental factors: Wind, smoke, and dry climates can exacerbate dry eye symptoms.
- Screen time: Prolonged use of computers, smartphones, and other screens can reduce blink rate, leading to dryness.
- Medications: Certain medications like antihistamines, decongestants, and antidepressants can reduce tear production.
- Medical conditions: Autoimmune diseases like Sjogren’s syndrome, rheumatoid arthritis, and lupus can cause dry eyes.
- Hormonal changes: Particularly in women, hormonal changes due to pregnancy, menopause, or oral contraceptives can affect tear production.
- Contact lenses: Wearing contact lenses can contribute to dry eyes.
- LASIK surgery: Post-surgery, some patients experience temporary or permanent dry eyes.
Symptoms
The symptoms of dry eye syndrome can vary in severity and may include:
- Redness: Often mistaken for conjunctivitis.
- Irritation: A burning or gritty sensation in the eyes.
- Excessive tearing: Reflex tearing due to irritation.
- Stringy mucus: Around or in the eyes.
- Blurred vision: Especially after periods of intense focus, like reading or screen use.
- Eye fatigue: Tired eyes, particularly after prolonged activities that require visual concentration.
- Sensitivity to light: Photophobia is common.
- Discomfort with contact lenses: Increased irritation when wearing lenses.
Diagnosis
Diagnosing dry eye syndrome involves several tests and examinations:
- Schirmer test: Measures tear production using a small strip of paper placed under the lower eyelid.
- Tear breakup time (TBUT): Evaluates the stability of the tear film.
- Ocular surface staining: Uses dyes like fluorescein to highlight damage to the corneal surface.
- Meibomian gland evaluation: Checks the function of glands that secrete oils into the tears.
Treatment
Treatment for dry eye syndrome aims to manage symptoms and improve tear production or quality:
- Artificial tears: Over-the-counter lubricating eye drops can provide relief.
- Prescription medications: Such as cyclosporine (Restasis) or lifitegrast (Xiidra) to reduce inflammation and increase tear production.
- Punctal plugs: Small devices inserted into the tear ducts to reduce tear drainage.
- Warm compresses and eyelid massages: To improve the function of meibomian glands.
- Omega-3 supplements: May help improve tear quality.
- Environmental modifications: Using humidifiers and avoiding dry, windy environments.
- Lid hygiene: Regular cleaning of the eyelids can help reduce symptoms.
Prevention
Preventing dry eye syndrome involves lifestyle adjustments and proactive eye care:
- Take breaks from screens: Follow the 20-20-20 rule (every 20 minutes, look at something 20 feet away for at least 20 seconds).
- Maintain proper humidity levels: Use a humidifier in dry environments.
- Wear protective eyewear: To shield eyes from wind and dry air.
- Stay hydrated: Drink plenty of water throughout the day.
- Follow good eyelid hygiene: Regularly clean eyelids and remove makeup thoroughly.
FAQs
How can I tell if it’s pink eye or a stye?
Pink eye generally affects the entire eye, causing widespread redness, itching, and discharge. A stye, on the other hand, is a localized infection that causes a painful, red bump near the edge of the eyelid. The key difference is the presence of a distinct, tender lump in the case of a stye, whereas pink eye results in a more diffuse redness and irritation.
What are the key differences between iritis and pink eye?
Iritis involves inflammation of the iris and presents symptoms like severe eye pain, light sensitivity, blurred vision, and a small or irregular pupil. Pink eye, however, causes less severe symptoms such as itching, burning, and a gritty feeling in the eye, without significant pain or changes in pupil size. Prompt medical attention is crucial for iritis to prevent complications, while pink eye often resolves with minimal treatment.
Can wearing contact lenses cause keratitis?
Yes, improper use of contact lenses can lead to keratitis. This includes wearing lenses for too long, not cleaning them properly, or using contaminated lenses. Symptoms of keratitis include severe eye pain, redness, blurred vision, and light sensitivity. Proper lens hygiene and following replacement schedules are essential to prevent keratitis.
How do allergies mimic pink eye symptoms?
Allergies can cause allergic conjunctivitis, leading to symptoms similar to pink eye, such as redness, itching, and watery eyes. These symptoms are triggered by exposure to allergens like pollen, dust, or pet dander, and often occur alongside other allergy symptoms like sneezing and nasal congestion. Managing allergen exposure and using antihistamines can help alleviate these symptoms.
What steps can help prevent dry eye syndrome?
Preventing dry eye syndrome involves several proactive measures:
- Staying hydrated: Drink plenty of water daily.
- Taking breaks from screens: Follow the 20-20-20 rule to reduce eye strain.
- Using a humidifier: Maintain adequate humidity in your environment.
- Wearing protective eyewear: Shield your eyes from wind and dry air.
- Practicing good eyelid hygiene: Regularly clean your eyelids to prevent oil gland blockage.
Last Words
Conditions like allergies, blepharitis, styes, iritis, keratitis, and dry eye syndrome share symptoms similar to conjunctivitis, making misdiagnosis common. By recognizing the distinct characteristics and causes of these conditions, you can seek appropriate medical advice and treatment, ensuring better eye health and comfort.
Always consult with a doctor if you experience persistent or severe symptoms to receive the correct diagnosis and care.









